ABSTRACT
Background: Arsenic pollution in groundwater, used for drinking purposes, has been envisaged as a problem of global concern. Treatment options for the management symptoms of chronic arsenicosis are limited. Mitigation option available for dealing with the health problem of ground water arsenic contamination rests mainly on supply of arsenic safe water in arsenic-endemic region of Indo-Bangladesh subcontinent. Limited information is available regarding the long-term effect of chronic arsenic toxicity after stoppage of consumption of arsenic-containing water.
Objective: The current study was, therefore, done to assess, objectively, the effect of drinking arsenic safe water (
Results: Manifestations of various skin lesions and systemic diseases associated with chronic arsenic exposure were ascertained initially by carrying on baseline study on 208 participants in Nadia (Cohort-I, with skin lesion and Cohort-II, without skin lesion) using a scoring system, as developed by us, and compared objectively at the end of each year for 3 year follow-up period. All the participants who had arsenic contaminated drinking water source in their houses were supplied with arsenic removal filters for getting arsenic-free water during the follow-up period. In participants belonging to Cohort-I, the skin score was found to improve significantly at the end of each year, and it was found to be reduced significantly from 2.17 ± 1.09 to 1.23 ± 1.17; P
Conclusion: It is, therefore, an urgent need to make arrangement for availability of safe water source among the arsenic-affected people in the district. Many of the people in the affected villages are not aware of contamination of their home tube wells with arsenic. Awareness generation and motivation of the people for testing their drinking water sources for arsenic and environmental interventions like rain water harvesting, ground water recharge, and restricting excessive use of ground water for domestic and agricultural purposes are also important to prevent further exposure of arsenic to these people.
Keywords: Arsenic and safe water, arsenic and skin score, arsenic and systemic disease score, treatment of arsenicosis
Introduction
Arsenic pollution in groundwater, used for drinking purposes, has been envisaged as a problem of global concern. The main source of arsenic in nature is ground water from naturally arsenic occurring aquifers i.e. geogenic cause besides water the other sources areanthropogenic sources like from insecticides, pesticides, wood preservatives, copper smelting, manufacturing of glass, pigments and electronic components and small amount used in herbal and traditional medicines and natural sources like atmosphere, soils andsediments, aquatic environment, and in organisms.
Arsenic contamination in drinking water has been reported from many countries, but the severity of this contamination in India and Bangladesh is unprecedented. In India, occurrences of arsenic in groundwater have also been reported from Bihar,Jharkhand, Chhattisgarh, Uttar Pradesh, and Assam.. Today, in West Bengal, the arsenic contamination in ground water has been detected in 79 blocks in 8 districts of the state. Of these, the major affected districts are Malda, Murshidabad, Nadia, Burdwan, and North and South 24 Parganas. It is suspected that 6 million people are exposed to arsenic-contaminated ground water (>50 μg/l).[1] Acute symptoms of arsenic poisoning mayinclude diarrhea, vomiting, blood in the urine, cramping muscles, hair loss, stomach pain, and more convulsions. The organs of the body that are usually affected by arsenic poisoning are the lungs, skin, kidneys, and liver. The fi nal result of arsenic poisoning is coma to death. But, chronic arsenic poisoning (Arsenicosis), over and above pigmentation, keratosis, produces protean manifestations like weakness, chronic respiratory disease, peripheral neuropathy, liver fibrosis, peripheral vascular disease etc.[2,3] Chronic arsenicosis leads to irreversible damage in several vital organs, and arsenic is an established carcinogen. Chronic arsenic toxicity is associated with skin, lungs, kidney, and liver cancers. Despite the magnitude of this potentially fatal toxicity, there is no effective therapy for this disease; patients once affected may not recover, even after remediation of the arsenic-contaminated water. The need for an effective therapy for chronic arsenicosis is obvious.
Chelation therapy for chronic arsenic toxicity is thought to be the specific therapy for relief of systemic clinical manifestations and reduction of arsenic stores in the body, reducing subsequent cancer risk. Chelation therapy is presumed to be more effective polyneuropathy, chronic lung and liver disease, swelling of hands and legs, and defects of hearing and vision are less likely to respond to this therapy. Chelating agents like meso-2,3-dimercaptosuccinicacid (DMSA), sodium 2,3-dimercapto-1-propane sulfonic acid (DMPS) and d-penicillamine have frequently been considered for treatment of chronic arsenic toxicity. However, their usefulness as a standard method of treatment is yet to be established.[4,5] Anti-oxidants and vitamins are also been tried by some workers for the treatment of arsenicosis.[6] But, no authentic evidence on the basis of placebo-controlled trial has been available substantiating the efficacy.
Earlier, we reported decrement of clinical score of arsenicosis following drinking of arsenic-safe water in a hospital-based study on 10 patients of arsenicosis who were also given high protein diet.[4] In a community-based study, interventions by reducingsupply of arsenic-contaminated water in a Southern Thailand showed both regression and progression of skin lesion, though the majority of the subjects followed up remained the same.[7] However, no objective evaluation of decrement of skin scoreon intake of arsenic-safe water was done in that study. Further, no report is available in regard to change in systemic disease features following intake of arsenic-safe water in an arsenicendemic population.
The current study was, therefore, done to assess the effect of drinking arsenic-safe water (
Materials and Methods
Nadia district is one of the worst arsenic-affected districts of West Bengal where all its 17 blocks are affected by ground water arsenic contamination. Manifestations of various skin lesions and systemic diseases associated with chronic arsenic exposure were ascertained initially by carrying on baseline study on 208 participants in Nadia (Cohort-I, with skin lesion and Cohort-II, without skin lesion) using a scoring system, as developed by us[4,8] and compared objectively at the end of each year for 3 year followupperiod. All the participants who had arsenic-contaminated drinking water source in their houses were supplied with arsenic removal filters for getting arsenic-free water during the follow-up period. Continuous monitoring of arsenic level in drinking water source and their morning urine samples for arsenic was also done at the end of each year of study. Photographic recording of skin lesions of each participant at baseline and 1st and 2nd and 3rd year follow-up study period was also done to objectively record the changes of skin score in time, if any.
Approval of the study protocol was obtained from the ethical committee of the foundation, fulfi lling the Helsinki criteria and recommendation of Indian Council of Medical Research, Govt. of India. All the participants gave their written consent for undergoing this study including taking photograph of their skin lesion.
Field study
Information from each recruit was collected on demographic and social characteristics and addiction to smoking, alcohol, or chewing tobacco with betel nut. Weight and height weremeasured, and Body Mass Index (BMI) was calculated (Weight in Kg/Height in meter[2]). All the participants were clinically examined including examination for typical arsenical skin lesion of pigmentation and/or keratosis and recording of bloodpressure was done. The patients were evaluated by an objective scoring system before and after every year of intake of arsenicsafe water. Skin scoring and systemic scoring were done as per standardized protocol described earlier.[4,8] Briefly, though manysymptomatic parameters recorded were subjective, the objective parameters included were pigmentation, keratosis, chest signs (rales and rhonchi), hepatomegaly, and splenomegaly. Flushing of face, solid edema of legs and hands, ascites, and absence deep reflexes for neuropathy were also included in the scoring system. Breathlessness at accustomed exertion, mild exertion, or at rest was defined as mild (1), moderate (2), and severe (3), respectively. Skin scoring was done based on mild, moderate, and severe lesionof pigmentation and keratosis.
Measurement of exposure
All exposed participants were questioned on lifetime history of water consumption using a structured questionnaire. Questions were asked as to sources of drinking and cooking water, and duration of water use from each source. Water samples were collected from present drinking and cooking water source of each participant and also from previous water sources when they were still available, in a polyethylene bottle from participants belonging to both the groups. Duration of intake of water from each water source was recorded.
First morning, void urine sample was also collected from participants in a container. Both the water and urine samples were kept in ice box before shifting from the field and stored at –20°C. For collection of hair, a bunch of whole length hair sample wascut from the scalp of each participant by a stainless blade and kept in a plastic packet. All these samples were stored according to standard protocol of WHO (2005)[9] until further analysis.
Arsenic levels in urine, hair, and water were measured using an atomic absorption spectrophotometer with a flow-injection hydride generation system as described by Das et al. (1995).[10] The limit of detection determined at the 90% confidence levelwas 3 μg/L. Hair samples were thoroughly cleaned and prepared in order to minimize the risk of surface contamination.
Results
There was no difference in regard to age and sex and BMI between the participants belonging to Cohort-I (arsenic-exposed with skin lesion) and Cohort-II (arsenic-exposed without skin lesion). There was also no difference between the peak and duration of arsenic exposure between the above two groups.
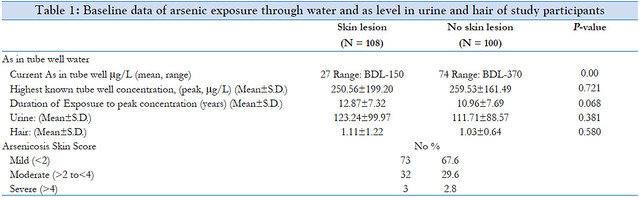
The mean peak (highest) arsenic level in drinking water of Cohort-I and Cohort-II participants was 250.56 ± 199.20 μg/L and 259.53 ± 161.49 μg/L, respectively. The mean duration of peak arsenic exposure of Cohort-I and Cohort-II participants was 12.87 ± 7.32 and 10.96 ± 7.69 years, respectively. The mean arsenic level in urine in Cohort-I and Cohort-II participants was 123.24 ± 99.97 μg/L and 111.71 ± 88.57 μg/L, respectively, and in hair,1.11 ± 1.22 mg/Kg and 1.03 ± 0.64 mg/Kg, respectively. There was no difference between mean arsenic level in biomarkers like urine (P = 0.3) and hair (P = 0.6) among both the cohorts [Table 1].
Out of the 108 Cohort-I cases, arsenical pigmentation and keratosis were present in 107 and 67 cases, respectively. According to total skin score, arsenical skin lesions were mild (≤2) in 73 (67.6%), moderate (>2 and ≤4) in 32 (29.6%), and severe (>4 and ≤6) in 3 (2.8%) arsenicosis cases [Table 1]. Though initial baseline study could be done on 108 participants of Cohort-I, the study could be repeated on 102 participants at the end of 1 year and on 100 participants at the end of 2nd year and 96 at the end of 3rd year. Out of 100 participants among Cohort-II in the baseline study, 98, 96, and 90 participants could be examined at the end of 1st, 2nd, and 3rd year follow-up study in successive years. In participants belonging to Cohort-I, signifi cant (P = 0.0097) improvement in skin score was observed 1 year after taking safe water (1.75 ± 1.24) in comparison to baseline value (2.17 ± 1.09). Further improvement in skin changes continued to occur in second (1.45 ± 1.19, P = 0.0000) and third year (1.23 ± 1.17, P = 0.0000) follow-up study.
In participants belonging to Cohort-I, the skin score was found to improve significantly at the end of each year, and it was found to be reduced significantly from 2.17 ± 1.09 to 1.23 ± 1.17; (P
Most important observation during the follow-up study was persistence of severe symptoms of chronic lung disease and severe skin lesion including Bowen’s disease in spite of taking arsenic-safe water in severe cases. Two participants died due to lung cancer and two due to severe lung disease associated with skin manifestations of arsenicosis during this period of follow-up study.
Discussion
This study describes demographic characteristics, clinical profile, and impact of drinking safe water (As level
In participants belonging to Cohort-I, the skin score was found to improve significantly at the end of each year, and it was found to be reduced significantly from 2.17 ± 1.09 to 1.23 ± 1.17;
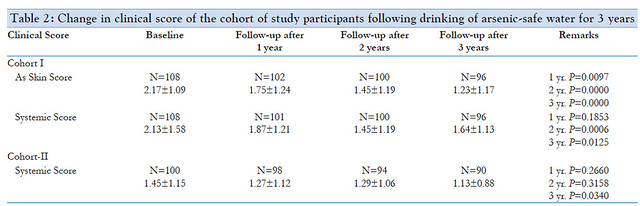 P
P Limited information is available in the literature regarding the long-term effect of chronic arsenic toxicity after stoppage of consumption of arsenic-containing water. To determine theeffect of providing safe water to affected people, a cohort of 24 patients with chronic arsenicosis were re-examined after drinking arsenic-free water ([11] These people had been drinking arsenic-contaminated water (130-2000 μg/l) for 4-15 years. Weakness and anemia were present in 91.6% and 58.3% of cases initially and were persistent in 60.8% and 33% of cases, respectively, on repeat examination. Partial improvement of pigmentation and keratosis were observed in 45% and 46% of patients, respectively. However, liver enlargement was persistent in 86% of cases. The most distressing observation was the new appearance of signs of chronic lung disease (cough, shortness of breath, and chest signs) in 41.6% of cases. There was a slight reduction of clinical symptoms of neuropathy. It was present in 11 cases (45.8%) at the time of initial examination and in 8 cases (33.8%) during the subsequent period (P [11]
Changes of severity of skin lesions over a period of 10 years were investigated amongst an affected cohort in an area having arsenic-contaminated shallow wells due to tin mining activities in Southern Thailand where interventions to reduce arseniccontaminated water had been implemented. Over 10-year period, both regression and progression of lesions occurred, though the majority of the subjects followed up remained the same. Drinking predominantly arsenic-free water increased the probability of regression in subjects with mild stage lesions but not in those with more advanced stage lesions. By contrast, a high arsenic content in the household well water, even though it was not used for drinking, decreased the probability of lesion regression among the subjects in more advanced stage but notamong milder stage cases. Irrespective of initial stage, a period of absence from the affected area increased the likelihood of lesion regression.[7]
Another cohort follow-up study was carried out by Guha Mazumder et al. (2003)[12] on 1074 people (arsenic-exposed people-623, control population-451) in South 24 Parganas,West Bengal, 5 years after an original baseline clinical examination. Out of 199 people with skin lesion among the arsenic-exposed population who were consuming safe waterduring the last 5 years, the skin lesions cleared or decreased in 49.7% of people. However, new skin lesions appeared in 32 (10.5%) out of 306 people who were not diagnosed with such lesions previously.
In a study carried out in Inner Mongolia, China, Sun et al. (2006)[13] reported that skin lesions improved to some extent after drinking low arsenic-containing water for 1 year. However, a 5-year follow-up study showed no more signifi cant improvement ofskin lesions, while the potential risk of arsenic-induced cancers after cutting off high arsenic exposure was still uncertain and indefinite.
The current study, for the first time, documented with sequential photographic records that arsenical skin lesions improve with intake of arsenic-safe water. However, it needs to be mentioned that improvement in skin score noticed were due to clearance of mild skin lesions (skin score 1-2), which were present in 67% of participants in the present study. But, in an endemic situation of ground water arsenic contamination of a country like West Bengal, the prevalence of arsenical skin lesions are mild (skin score 1-2) in majority (87.56%) of the cases.[5] Hence, the main strategy for arsenic mitigation program need to beaddressed to ensure availability of arsenic-safe water in an arsenic-endemic region.
However, the prognosis of arsenicosis cases with severe skin lesion and major systemic disease like chronic lung disease are unsatisfactory, and fatality occurs due to severe lung disease and cancers, like lung cancer.
Conclusion and Recommendation
Intervention with arsenic-safe water was found to cause improvement of skin score in signifi cant number of cases of arsenicosis with skin lesion. However, systemic score showed milder improvement in both arsenic-exposed people with and without skin lesion. Symptoms of severe skin lesion and Bowens persisted. Both cancer and non-cancer causesof death due to involvement of lung were found to be the major causes of mortality in arsenic-exposed study people in Nadia. The primary care providers of the local region canidentify the problem early and can start prompt intervention to prevent development of future complication of chronic arsenic toxicity like cancers and other systemic complications.Despite the magnitude of this potentially fatal toxicity, there is no effective therapy for this disease; patients once affected may not recover. Only cessation of exposure to drinking water or items of elevated concentration of arsenic was believed to provide effective remedy. So, primary prevention by raising levels of awareness among primary care providers of the local region about signs and symptoms of arsenicosis and available intervention will definitely help to mitigate this important public health problem.
It is, therefore, an urgent need to make arrangement for availability of safe water source among the arsenic-affected people in the district. Many of the people in the affected villagesare not aware of contamination of their home tube wells with arsenic. Awareness generation and motivation of the people for testing their drinking water sources for arsenic and environmental interventions like rain water harvesting, ground water recharge,and restricting excessive use of ground water for domestic and agricultural purposes are also important to prevent further exposure of arsenic to these people.
Further, arsenic-affected people with severe skin lesions and systemic manifestations like lung disease, neuropathy etc. are having unbearable suffering. These people are very poor and live in distant villages where hospital facilities are not easily available. Arrangement for free treatment of these patients in state referral hospitals and free transport facility from theirvillages could help a lot in alleviating the suffering of these people.
References
1. IARC. Some drinking-water Disinfectants and contaminants, including Arsenic. Monographs on the Evaluation of Carcinogenic risks to Humans. Vol. 84. Lyon, France: WHO; 2004. p. 61-96.
2. Guha Mazumder DN, Haque R, Ghosh N, De BK, Santra A, Chakraborty D, et al. Arsenic levels in drinking water and the prevalence of skin lesions in West Bengal, India. Int JEpidemiol 1998;27:871-7.
3. Haque R, Mazumder DN, Samanta S, Ghosh N, Kalman D, Smith MM, et al. Arsenic in drinking water and skin lesions: Dose-response data from West Bengal, India. Epidemiology2003;14:174-82.
4. Guha Mazumder DN. Criteria for case definition of arsenicosis. Arsenic Exposure and Health Effect V. In: Abernathy CO, Calderon RL, Thomas and DL, Chappell WR,editors. London: Chapman and Hall; 2003. p. 117-33.
5. Majumder KK, Guha Mazumder DN, Ghose N, Lahiri S. Systemic manifestations in chronic arsenic toxicity in absence of skin lesions in West Bengal. Indian J Med Res 2009;129:75-82.
6. Guha Mazumder DN, Das Gupta J, Santra A, Pal A, Ghose A, Sarkar S. Chronic arsenic toxicity in West Bengal – The worst calamity in the world. J Indian Med Assoc 1998b;96:4-7.
7. Guha Mazumder DN, Haque R, Ghosh N, Dey BK, Santra A, Chakraborti D, et al. Arsenic in drinking water and the prevalence of respiratory effects in West Bengal, India. IntJ Epidemiol 2000;29:1047-52.
8. Guha Mazumder DN, Ghosh A, Majumdar KK, Ghosh N, Saha C, Mazumder RN. Arsenic Contamination of ground water and its health impact on population of district of Nadia,West Bengal, India. Indian J Community Med 2010;35:331-8.
9. WHO. Technical Publication No. 30. Clinical aspects of Arsenicosis. A Field Guide for Detection, management and surveillance of arsenicosis cases. In: Caussy D, editor. NewDelhi: WHO Regional Office for South East Asia; 2005. p. 5-9.
10. Das D, Chatterjee A, Samanta G, Mandal B, Chowdhury TR, Samanta G, et al. Arsenic contamination in groundwater in six districts of West Bengal, India: The biggest arseniccalamity in the world. Analyst 1994;119:168N-70.
11. Guha Mazumder DN, De BK, Santra A, Gupta JD, Ghosh N, Roy BK, et al. Chronic arsenic toxicity: Epidemiology, natural history and treatment. In: Chappell WR, Abernathy CO, Calderon RL, editors. Arsenic exposure and health effects. London, UK: Elsevier; 1999. p. 335-47.
12. Haque R, Guha Mazumder DN, Samanta S, Ghosh N, Kalman D, Smith MM, et al. Arsenic in drinking water and skin lesions: Dose-response data from West Bengal, India.Epidemiology 2003a;14:174-82.
13. Sun G, Li X, Pi J, Sun Y, Li B, Jin Y, et al. Current Research problems of chonic arsenicosis in China. J Health Popul Nutr 2006;24:176-81.
Department of Community Medicine, KPC Medical College and Hospital, Jadavpur, Kolkata, DNGM Research Foundation, Kolkata, India
Posted by













